Colleagues from Oxford Health Research & Development team are attending the International Mental Health Nursing Research Conference, a knowledge sharing event dedicated to research in mental health nursing.
Debbie Moll, Research Speech and Language Therapist in the Memory and Cognition research delivery team and Patient and Public Involvement Lead at the OH CRF, along with Jemima Littlejohns, Research Training and Development Manager at Oxford Health will present findings from the CoDAQ study, which looked into improving communication in people with dementia.
The 29th International Mental Health Nurse Research Conference will take place on Thursday 12 and Friday 13 September at St Catherine’s College, Oxford.
Please see the Mental Health Nurse Academics UK website for more information.











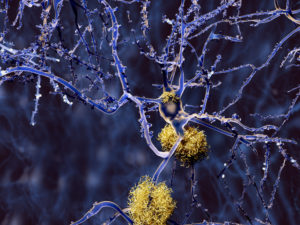
 Alzheimer’s disease creeps up on us so slowly that the amazing capacity of the brain to adapt means we literally do not notice. Research has shown that this period – when the process of Alzheimer’s pathology has started in the brain but there is no apparent effect on the person – lasts for 10, maybe even 20 years. We call this the preclinical period. Given that Alzheimer’s disease becomes common after people reach their mid 70’s, then the man in his 50’s who I live with may just be beginning to have the very first changes in his brain, even if he doesn’t know it.
Alzheimer’s disease creeps up on us so slowly that the amazing capacity of the brain to adapt means we literally do not notice. Research has shown that this period – when the process of Alzheimer’s pathology has started in the brain but there is no apparent effect on the person – lasts for 10, maybe even 20 years. We call this the preclinical period. Given that Alzheimer’s disease becomes common after people reach their mid 70’s, then the man in his 50’s who I live with may just be beginning to have the very first changes in his brain, even if he doesn’t know it.